| |
Oral Cholesterol Lowering Drugs
|
|
|
|
Hypercholesterolaemia
|
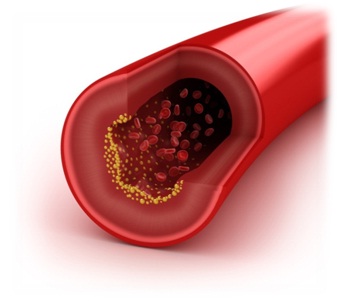
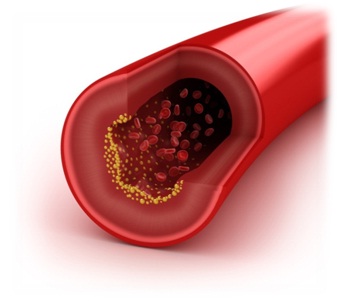
Cholesterol is a fat-like substance found in your body and it is mainly made by
the liver or absorbed via food intake. Being insoluble in water, cholesterol binds
to proteins to become lipoproteins so that it can be transported in blood. There
are different types of lipoprotein cholesterol, depending on the proportion of cholesterol,
triglyceride, etc. the lipoprotein carries. Two most commonly known types of lipoprotein
cholesterol are:
- High-density lipoprotein (HDL) cholesterol– also known as “good cholesterol”. It
carries excess cholesterol back to the liver for degradation or excretion.
- Low-density lipoprotein (LDL) cholesterol- LDL cholesterol or “bad cholesterol”
carries cholesterol around your body. Excess cholesterol will build up in the walls
and clog the arteries.
|
|
|
|
Whilst cholesterol is essential for building cells and producing hormones in the
body, having high level of bad cholesterol in your blood (hypercholesterolaemia)
can increase your risk of developing cardiovascular diseases, e.g. heart attack
or stroke. Thus, maintaining your cholesterol level at healthy level can reduce
your risk of developing cardiovascular diseases.
There are many factors associated with high blood cholesterol which include older
age, unhealthy diet, obesity, lack of exercise, drinking excessive amount of alcohol,
smoking and family history of hypercholesterolaemia. Furthermore, some kidney and
liver diseases or underactive thyroid glands can also raise blood cholesterol levels.
Patients suffering from hypercholesterolaemia usually have no symptoms and a simple
blood test can confirm the diagnosis.
|
|
▲ back to top
|
Treatment
|
The aim of treatment for hypercholesterolaemia is not merely to lower your cholesterol
level but also to control your risk of developing cardiovascular diseases. For patients
who have high blood cholesterol, if you do not have heart disease or secondary causes
for hypercholesterolaemia, you will usually be advised to make lifestyle changes
first such as regularly exercising more and eating a healthier diet. If your cholesterol
level does not improve after a few months and your estimated risk of developing
cardiovascular diseases is high, your doctor may recommend you to take cholesterol
lowering drugs in addition to dietary and lifestyle modifications.
|
|

|
|
▲ back to top
|
Cholesterol Lowering Drugs
|
In Hong Kong, most cholesterol lowering drugs can only be obtained from pharmacy
with a prescription. They should be used under close supervision by healthcare professionals.
Commonly used cholesterol lowering drugs include statins, fibrates, bile-acid binding
resins, ezetimibe and nicotinic acid.
|
|

|
1. Statins (e.g. lovastatin, simvastatin, atorvastatin, rosuvastatin)
Statins reduce the production of cholesterol by the liver and this causes your liver
to absorb cholesterol from your blood. They are generally considered to be the most
effective type of cholesterol lowering drugs. Statins may also be used to reduce
your risk of developing cardiovascular diseases.
Statins may affect liver function. If you have liver disease or persistently abnormal
liver function tests, you should not take statins. Before you start taking a statin,
your doctor may order a blood test to ensure your liver function is normal. These tests
may be repeated regularly whilst you are taking these medicines to monitor your liver
function. Furthermore, statins may cause inflammation and damage to your muscles,
especially if they are given at a high dose or in conjunction with certain drugs such as
itraconazole, ketoconazole, erythromycin, gemfibrozil, etc. There could also be muscle
pain; and in rare cases, there could be serious and acute manifestation of the muscle
damage (e.g. rhabdomyolysis). You should always follow the dosage recommended by your
healthcare professionals and report any symptoms to your doctors.
Lovastatin is one of the earliest marketed statins. It was synthesized chemically and
marketed as a western medicine to reduce blood cholesterol in the 80’s. However, it was
later found that its chemical structure is the same as a compound called monacolin K found
in red yeast rice. Red yeast rice (abbreviated: RYR; sometimes known as: red fermented
rice; Chinese name: 红麴米/红麴/红曲/赤曲/丹曲, is obtained by fermenting rice with some kinds of
fungi (e.g. Monascus purpureus). After fermentation, many active natural substances will be
produced in the RYR, including monacolin K (shown in the figure) which is an active substance
with a lipid lowering potency. In other words, the RYR contains lovastatin (i.e. monacolin
K); but as the amount of lovastatin in the RYR varies significantly, it is not recommended
as a medicine for treating hypercholesterolaemia.
.png)
If your blood lipid level cannot be controlled by statins, addition of other cholesterol
lowering drug may be needed but close medical supervision is required because of
possible drug interactions.
2. Bile-acid binding resins (e.g. colestyramine)
The body makes bile acids by breaking down LDL cholesterol. Bile-acid binding resins
lower LDL cholesterol by combining with bile acids, preventing their intestinal
reabsorption, so that your liver needs to break down cholesterol from your blood
to produce bile acids.
3. Ezetimibe
Ezetimibe blocks the intestinal absorption of dietary cholesterol into your blood,
thus lowering your cholesterol level. It is used as an adjunct to dietary modification
in patients with primary hypercholesterolaemia and patients with homozygous familial
hypercholesterolaemia in combination with a statin.
4. Fibrates (e.g. bezafibrate, fenofibrate, gemfibrozil)
Fibrates reduce triglycerides and increases level of HDL cholesterol in your blood.
They are used mainly in patients with hypertriglyceridaemia. Patients with hypercholesterolaemia
can change to take fibrates when a statin is contraindicated or not tolerated.
5. Nicotinic acid
Nicotinic acid decreases LDL cholesterol whilst increases HDL cholesterol levels
in your blood. However, its clinical use is limited by the side effects of vasodilatation
and possible risk of liver damage with long term use.
|
|
▲ back to top
Common Side Effects and Precautions
Common side effects and precautions in taking cholesterol lowering drugs are:
|
Types of cholesterol lowering drugs
|
Common side effects
|
Precautions
|
|
1. StatinsΔ
|
Gastrointestinal discomfort, headache, muscle pain, abnormal liver function. Rarely,
patients may develop myopathy or rhabdomyolysis (muscle disorders that cause breakdown
of muscles and lead to muscle pain); and cognitive impairment (e.g. memory loss,
forgetfulness, state of confusion)
|
- not suitable in patients with liver disease or persistently abnormal liver function
test
- not suitable during pregnancy or while breastfeeding
- take the medicine in the evening*
- avoid large quantities of grapefruit juice as it may increase your risk of developing
side effectΦ
- statins should be taken with caution for patients at risk of having myopathy or
rhabdomyolysis. Contact your doctor immediately if you experience muscle pain,tenderness
or weakness
- statins may interact with other drugs such as cardiovascular drugs, antimicrobials
and drugs used in treating AIDS or hepatitis C which could increase the level of
statins in the body, thus increasing their risk of causing side effects.
|
|
2. Bile-acid binding resins
|
Gastro-intestinal discomfort, constipation, nausea,may increase triglyceride levels
and aggravate hypertriglyceridemia.
|
- should be mixed with about 150ml of a suitable liquid, such as water or fruit juice,
before taking
- should have high fibre diet and drink plenty of fluid to reduce the side effect
of constipation
- other drugs should be taken at least 1 hour before or 4-6 hours after to reduce
possible interference with absorption
- may interfere the absorption of fat-soluble vitamins and vitamin supplements (e.g.
A, D and K)may be required for prolonged use
- should be used with caution during pregnancy as they may cause fat soluble vitamins
deficiency with prolonged use
|
|
3. Ezetimibe
|
abdominal pain, diarrhea, headache, fatigue, muscle pain
|
- safe use has not been established during pregnancy and ezetimibe should only be
used if benefits outweigh risks.
- should avoid in patients with moderate or severe hepatic impairment
|
|
4. Fibrates
|
Gastro-intestinal discomfort including nausea and anorexia, rash, vertigo, headache
|
- contact your doctor immediately if you experience muscle pain, tenderness or weakness
- may cause dizziness, if affected, patients should not drive or operate machinery
- if you are pregnant, please seek advice from your doctor on the most appropriate
choice of medications.
|
|
5. Nicotinic Acid
|
Facial and neck flushing, nausea, vomiting, diarrhea. Taking high dose for long
time could also lead to liver damage
|
- avoid during pregnancy or while breastfeeding
- monitoring of liver function is required
- may be associated with myopathy when used with statins
|
* Except for rosuvastatin and atorvastatin which can be taken at
any time during the day
Φ Except for rosuvastatin which is not a substrate for the enzyme
inhibited by grapefruit juice
Δ The side effects of statin may also be applicable to the RYR
which contains lovastatin
|
▲ back to top
|
General advice on taking cholesterol lowering drugs
|
-
Cholesterol lowering drugs (e.g. statins, fibrates, ezetimibe, nicotinic acid)
are prescription medicines and should only be purchased with a doctor’s
prescription and taken as directed by your doctor.
-
Be familiar with the name and dosage of the drugs you are taking. Be cautious about
their possible side effects.
-
Cholesterol lowering drugs are normally to be taken in the evening.
-
RYR, presented as food supplement, may contain variable amount of the substance lovastatin.
Be aware of its add-on effect on medications (including on other statins) such as the development of any signs of muscle pain.
-
Have regular tests for the cholesterol and liver function as prescribed by your doctor.
|
|
▲ back to top
|
Communication with your doctor
|
|
-
Seek your doctor’s advice on the best treatment option. There are many types of
cholesterol lowering drugs with different actions and side effect profiles; your
doctor will use the most appropriate drugs after considering your condition and
your response to the drugs.
-
Inform your doctor of your medical history and the drugs you are taking because
other drugs may interact with cholesterol lowering medications and some disease
may warrant special precautionary measures.
|
 |
-
Inform your doctor that you are pregnant or breast feeding as some types of cholesterol
lowering drugs should not be taken by women who are pregnant or breast feeding.
-
Seek medical advice as soon as possible if you experience any side effects suspected
to be related to your cholesterol lowering drugs, such as muscle pain, tenderness
and weakness.
-
Have regular follow-ups as advised by your doctor.
|
|
|
|
-
Ask your doctor before taking any other medicines or health products (e.g. RYR)
as they may affect the effect of your medication. Don't control your cholesterol
by self-medicating health products solely relying on the product claims. In fact,
products that claimed to stabilize cholesterol and blood lipids have previously
been found to be adulterated with cholesterol lowering drug ingredients.
|
|
|
|
|




.png)

