| |
| |
Anti-Asthmatic Drugs
|
|
 |
Preface
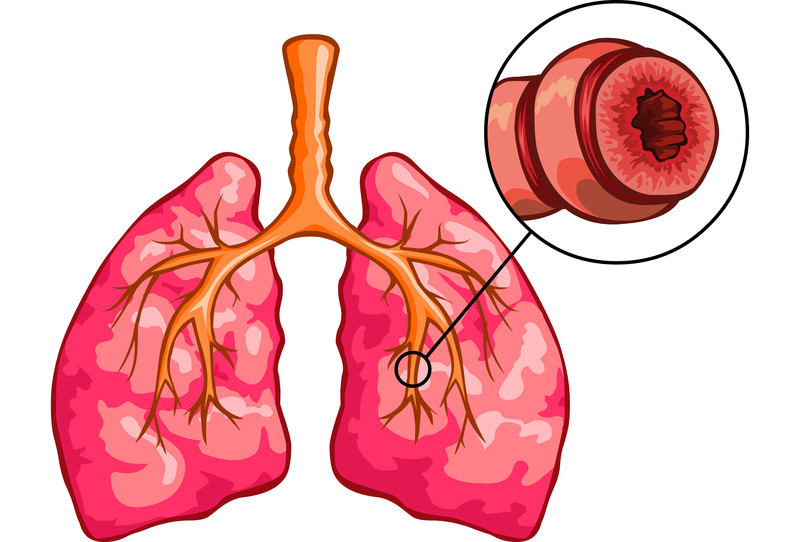
Asthma is a chronic disease that inflames the airways (i.e. the small tubes, called bronchi) which carry air in and out of the lungs. In asthmatic patient, the bronchi will be inflamed and more sensitive than normal and produce extra mucus. This can make breathing difficult due to reversible airflow obstruction, or bronchospasm, and trigger coughing, wheezing and shortness of breath.
|
|
 |
|
The cause of asthma is not fully understood, but it’s probably due to a combination of the following factors:
|
|
Environmental: allergens (e.g., house dust mites, animal fur and pollen), occupational irritants, tobacco smoke, respiratory (viral) infections, strong emotional expressions and drugs (e.g. aspirin and beta blockers).
|
|
Genetic (inherited): usually occurs in children. The chances of developing asthma are increased if the patients’ family members or relatives have asthma and other allergic conditions such as atopic dermatitis and hay fever.
|
|
▲ back to top
Treatment
There are a number of treatments that can help effectively control or sooth the asthmatic condition. Treatment is based on two important goals which are (i) specific regimens for the treatment of acute attacks by opening swollen airways that are limiting breathing, and (ii) prophylactic measures to reduce inflammation and airway resistance and to maintain airflow. Treatment and prevention involves a combination of medicines, lifestyle advices, and identifying and then avoiding potential asthma triggers.
|
|
Drugs which are indicated for the treatment of asthma include the classes of beta2 agonists, antimuscarinics, corticosteroids, leukotriene inhibitors and xanthines. They are available in the forms of inhalations, tablets, capsules and injections, etc. and used depending on medical condition and supervision.
|

|
Inhalation preparations include solutions for nebulisation, metered-dose inhalers, and powdered inhalers. Asthma medicines are usually given by inhalers, which are the devices that deliver the drug directly into the airways through your mouth when you breathe in. Using an inhaler is the most common and effective way of taking asthma medicines as it goes straight into your lungs. However, each inhaler works in a slightly different way. Some inhalers emit an aerosol jet when pressed. They work better if given through a spacer, which is a plastic or metal container with a mouthpiece at one end and a hole for the inhaler at the other. It traps the medicine inside the spacer, so you don't have to worry about pressing the inhaler and breathing in at exactly the same time.
|
|
Majority of the products are prescription-only medicines and should be used strictly under doctor’s instruction and recommendation. Others, such as inhalers from some of the beta2 agonists and corticosteroids classes, can be purchased from registered pharmacies under the supervision of a registered pharmacist.
|
|
|
▲ back to top
|
Drugs for treating asthma are divided into two categories: (1) Quick-relief medications (which are used to relief acute asthma) and (2) Long-term asthma control medications with (which are used as prophylactic measures) details below:-
|
| 1. |
Quick-relief medications: they are used as needed for rapid, short-term symptom relief during an asthma attack. Types of quick-relief medications are: |
| |
| a. | Short-acting beta2 agonists: these inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms during an asthma attack. Short-acting beta2 agonists can be taken using a portable, hand-held inhaler or a nebulizer. Examples are salbutamol and terbutaline. |
| b. | Antimuscarinics: these inhaled antimuscarinics act quickly to immediately relax the airways, like other bronchodilators, making it easier to breathe. Examples are ipratropium and tiotropium. |
| c. | Systemic corticosteroids: these systemic corticosteroids (i.e., oral and intravenous routes) relieve airway inflammation caused by severe asthma. However, due to serious side effects when used long term, the systemic routes are used only on a short-term basis to treat severe asthma symptoms. Examples are prednisone and methylprednisone. |
| d. | Intravenous xanthines: these xanthines relax smooth muscle and to relieve bronchial spasm and are indicated for severe asthma attack. Example is aminophylline. |
|
|
 |
| 2. |
Long-term asthma control medications: they work to reduce the amount of inflammation in the airways and prevent asthma attacks occurring. |
| |
| a. | Inhaled corticosteroids: they are the most effective preventers, however, you may need to use these medications for several days to weeks before they reach their maximum benefit. Examples are fluticasone and budesonide. |
| b. | Long-acting beta2 agonists: these inhaled medications open the airways. Some research shows that they may increase the risk of a severe asthma attack, unless they are used in combination with an inhaled corticosteroid. Examples are salmeterol and formoterol. |
| c. | Leukotriene inhibitors: they act against one of the inflammatory components of asthma and provide protection against bronchoconstriction when taken before exercise or exposure to allergen or to cold air. Examples of leukotriene inhibitors include montelukast and zafirlukast. |
| d. | Xanthines: apart from relaxation of bronchial muscle and relief of bronchial spasm, they can stimulant effects on respiration and have anti-inflammatory effects. Example is theophylline. |
|
|
|
▲ back to top
Common side effects and Precautions |
Types of Anti-Asthmatic Drugs
|
Common side effects
|
Precautions
|
|
1. Beta2 agonists |
- Fine tremor (particularly in the hands)
- Nervous tension
- Headache
- Muscle cramps
- Palpitation
|
- Should be used with caution in patients with hyperthyroidism, cardiovascular disease, arrhythmias, susceptibility to QT-interval prolongation, and hypertension
- Should also be used with caution in diabetic patients - monitor blood glucose may be required due to the risk of ketoacidosis, especially when beta2 agonist given intravenously
|
|
2. Antimuscarinics |
- Dry mouth
- Gastro-intestinal motility disorder (including constipation and diarrhoea)
- Cough
- Headache
|
- Should be used with caution in patients with prostatic hyperplasia, bladder outflow obstruction, and those susceptible to angle-closure glaucoma
|
|
3. Corticosteroids |
|
a. Systemic corticosteroids |
- Fragile bones
- High blood pressure
- Diabetes
- Weight gain
- Cataracts and glaucoma
- Thinning of the skin
- Easy bruising
- Muscle weakness
|
- Initial growth velocity may be reduced in children with systemic corticosteroid therapy
- A potential for paradoxical bronchospasm
|
|
b. Inhaled corticosteroids |
- Fungal infection of the mouth or throat,
- May develop a hoarse voice
|
- Monitor the height and weight of children annually
- Association with adrenal crisis and coma in children, thus avoid excessive dose
|
|
4. Leukotriene inhibitors |
- Abdominal pain
- Thirst
- Headache
- Hyperkinesia (in young children)
|
- Should not be used for the treatment of acute asthma attacks
- Caution in pregnancy and breastfeeding
|
|
5. Xanthines |
- Nausea, vomiting
- Gastric irritation
- Diarrhoea
- Palpitation
- Tachycardia
- Arrhythmias
- Headache
- Insomnia
|
- Should be used with caution in patients with heart failure, hepatic impairment and viral infections
- Should also be used with caution in the elderly, smokers and alcoholics
- Should avoid the concurrent use of intravenous and other routes of administration of xanthines
|
|
|
▲ back to top
General advice on taking Anti-Asthmatic Drugs
Follow doctors’ instructions, and learn how to use the inhalers correctly. Do not stop or change the regimens by yourself, unless there is a self management plan agreed with your doctor. Discuss your difficulty if any with your doctor or pharmacist. You should use the reliever inhaler (used to relief acute asthma) followed by the preventer inhaler (used as a prophylactic measure) if you need to use both. You should carry your short-acting reliever inhaler with you at all times for acute asthma attack. If you need it more often than usual, you should see your doctor. Severe asthma patients should not take aspirin and anti-inflammatory painkillers without consulting doctors. Wash inhalers with lukewarm water and let it dry if nozzle is blocked. Rinse mouth after use of corticosteroid inhalers. Take the medications before bed to avoid asthma attack during sleep.
|
|
 |
|
▲ back to top
Communication with your doctor
|

|
Seek medical advice on the best treatment option. Your doctor will prescribe the most appropriate drugs for you after considering your condition and your response to the drugs. You may be prescribed more than one medication for treating asthma, make sure that you are aware of the purpose and usage of each preparation and consult your doctor if you have any doubts. Inform your doctor of the medicines you are taking, and of any diseases you are suffering as these may warrant special precautions to the use of anti-asthmatic drugs. Seek medical advice immediately if you experience any symptoms or side effects suspected to be related to anti-asthmatic drugs. Your doctor may review your medications. Have regular medical follow-ups as advised by your doctor if you need to use anti-asthmatic drugs on a long-term basis.
|
|
|
▲ back to top
Storage of Anti-Asthmatic Drugs
Anti-asthmatic drugs should be kept in a cool and dry place. Unless specified on the label, medicines should not be stored in refrigerators. Furthermore, drugs should be kept properly in places unreachable by children to prevent accidental ingestion.
|
|
▲ back to top
|
|
Acknowledgement : The Drug Office would like to thank the Professional Development and Quality Assurance (PD&QA) for their valuable contribution to the preparation of this article.
|
|
|
|
|


