| |
Oral Antiepileptic Drugs (AEDs)
|

|
Epilepsy
|
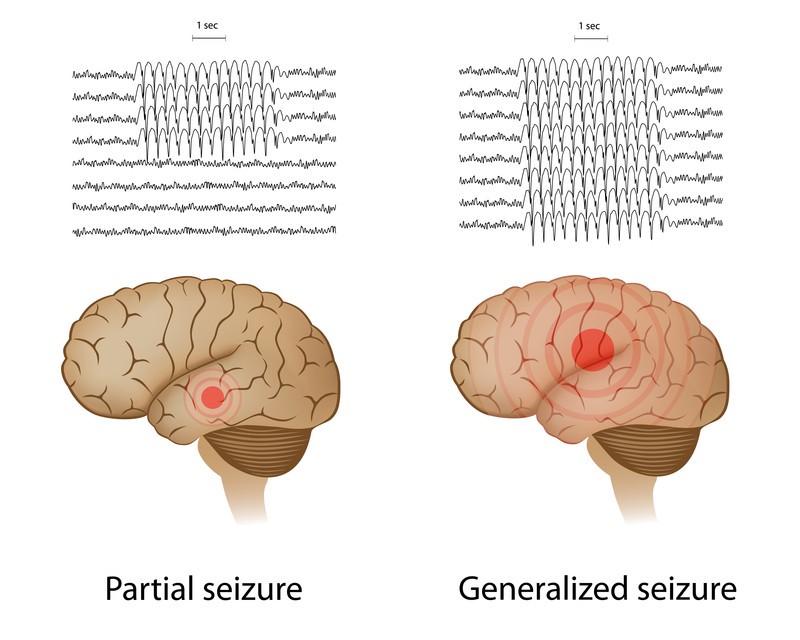
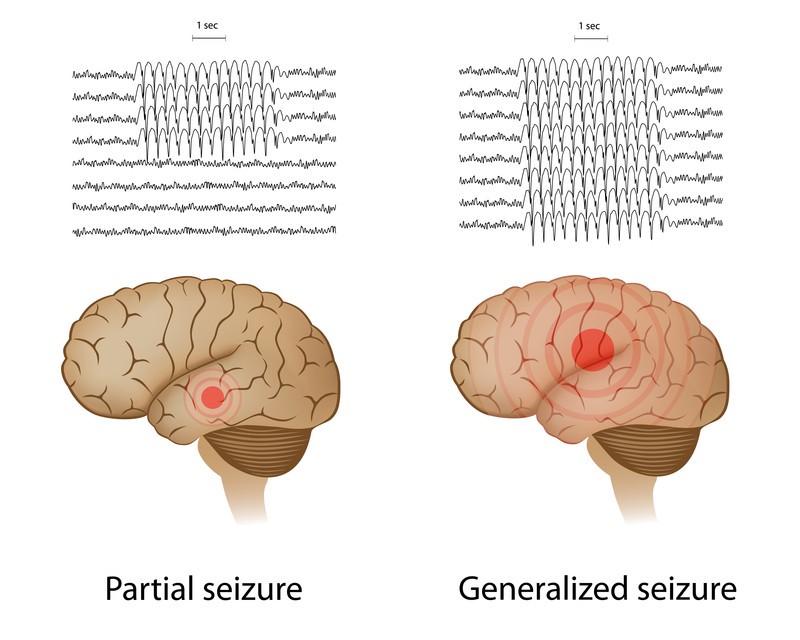
Epilepsy is a central nervous system disorder (neurological disorder) that causes people to have recurring seizures. The seizures happen when the nerve cell activity in your brain is disturbed, causing you to experience abnormal behaviour, symptoms and sensations, including loss of consciousness. An individual’s lifetime risk of developing epilepsy is between 3 and 5%; neonates, children, and the elderly are at the highest risk of developing the disorder.
|
| Epilepsy is generally classified into partial (focal) seizures which localized in one area of the brain at onset, and generalized seizure which involved both cerebral hemispheres simultaneously from the outset. Partial seizure may become secondary generalized seizures if the nerve cell activity spreads to involve the entire brain. Symptoms vary depending on the type of seizure, and may involve temporary confusion, a staring spell, uncontrollable jerking movements of the arms and legs, loss of consciousness or awareness, and psychic symptoms.
|
|
|
▲ back to top
Treatment |
|
Antiepileptic drugs (AEDs) are usually the first choice of treatment. AEDs do not cure epilepsy. About 70% of people with epilepsy have their seizures controlled with AEDs when they are taking the prescribed drugs regularly. If medications do not treat the condition, surgery or another type of treatment may be used as directed by doctors. Other treatments include vagus nerve stimulation (implant a small electrical device under your skin to pass electricity to stimulate the nerve), and ketogenic diet (a diet which is high in fats and low in carbohydrates and protein) which is sometimes advised for children.
|
All the registered AEDs in Hong Kong are available in oral dosage forms e.g. tablets, capsules, syrups and solutions. A few of them are also available in injectable forms. All these products are prescription-only medicines and should be administered strictly under doctor’s instruction and recommendation.
|
Classification of antiepileptic drugs (AEDs) |
Generally, AEDs work by changing the levels of the chemicals in your brain that conduct electrical impulse, and this reduces the chance of a seizure. The choice of antiepileptic is determined mainly by its efficacy against the type of seizures experienced and its potential adverse effects. Other factors such as concomitant medication, co-morbidity, age and sex would also be taken into account.
|
AED should be started using the lowest possible dose of a single drug in order to achieve maximum seizure control with minimum side effects. When monotherapy with a first-line AED failed, monotherapy with a second drug may be tried. If the condition does not improve, combination therapy with two or more AEDs may be necessary.
|
Different AEDs vary considerably in their characteristics, which influences the risk of whether switching between different manufacturers’ products of a particular drug may cause adverse effects or loss of seizure control. Therefore, AEDs have been divided into three risk-based categories:
|
- Category 1: It is advisable to maintain on a specific manufacturer’s product. Examples are carbamazepine, phenytoin, and phenobarbitone/phenobarbital.
- Category 2: The need for continued supply of a particular manufacturer’s product should be based on clinical judgment taking the factors such as seizure frequency and treatment history into account. Examples are oxcarbazepine, valproate, lamotrigine, clobazam, clonazepam, retigabine, and topiramate.
- Category 3: Usually unnecessary to maintain on a specific manufacturer’s product. Examples are gabapentin, pregabalin, vigabatrin, levetiracetam, and lacosamide.
|
|
|
▲ back to top
Common side effects and Precautions
Every AED can sometimes cause side effects of fatigue, dizziness, unsteadiness, blurry vision, stomach upset, headaches, memory and thinking problems. Weight gain tends to occur with valproate, gabapentin, pregabalin and carbamazepine. Weight loss tends to occur with topiramate.
|
Antiepileptic drug
|
Common side effects
|
Precautions
|
| Category 1 drug |
| 1. Carbamazepine |
- Headache, ataxiaΩ, drowsiness, dizziness, and unsteadiness,
- Nausea and vomiting
- Blurred vision
- Allergic skin reactions
|
- Use with caution with cardiac disease, skin reaction, impaired hepatic or renal function
- Test for HLA-B*1502 allele in individuals of Han Chinese or Thai origin#
- Contraindicated in cardiac conduction problem (unless paced); history of bone-marrow depression, and acute porphyriaΦ
- Seek immediate medical attention if symptoms such as fever, rash, mouth ulcers, bruising, or bleeding develop
|
| 2. Phenytoin |
- Headache, dizziness, tremor, transient nervousness, and insomnia
- Nausea, vomiting, and constipation
- Tenderness and hyperplasia of the gums
- Acne, hirsutismψ, and coarsening of the facial features
|
- Use with caution in patients with impaired liver function or diabetes
- Test for HLA-B*1502 allele in individuals of Han Chinese or Thai origin#
- Seek immediate medical attention if symptoms such as fever, sore throat, rash, mouth ulcers, bruising, or bleeding develop
|
| 3. | Phenobarbitone/ Phenobarbital |
|
- Drowsiness and lethargy
- Subtle mood changes
- Impaired memory and cognition
- Paradoxical excitement, restlessness, and confusion in the elderly, and irritability and hyperactivity in children.
- Nystagmusδ, ataxiaΩ and respiratory depression may occur at high dose
|
- Use with caution in elderly, debilitated people, children, patients with respiratory depression (avoid if severe), history of alcohol or drug abuse, or in renal impairment
- Avoid in porphyriaΦ, severe hepatic impairment, or in patients with a personal or family history of an affective disorder
|
| Category 2 drug |
| 4. Oxcarbazepine |
- Nausea, vomiting, constipation, diarrhea
- Dizziness, drowsiness, headache
- Agitation, confusion, amnesia, impaired concentration
- Nystagmusδ, visual disturbance
- Rash
|
- Use with caution in patient with hyponatraemia, heart failure, cardiac conduction disorder, or severe hepatic impairment
- Reduce dose in renal impairment
- Test for HLA-B*1502 allele in individuals of Han Chinese or Thai origin#
- Avoid in acute porphyriaΦ
|
| 5. Valproate |
- Nausea, gastric irritation, diarrhea
- Increased appetite and weight gain
- Hyperammonaemia, thrombocytopeniaχ
- Transient hair loss (regrowth may be curly)
|
- Contraindicated in patient with family history of severe hepatic dysfunction, or acute porphyriaΦ
- Avoid in hepatic impairment or acute liver disease
- Seek immediate medical attention if symptoms such as abdominal pain, nausea or vomiting develop
|
| 6. Lamotrigine |
- Nausea, vomiting, diarrhea
- Drowsiness, dizziness
- Insomnia
- Aggression, irritation
- Back pain, arthralgia
- AtaxiaΩ, nystagmusδ
- Diplopia, blurred vision
- Rash
|
- Use with caution in renal failure, or moderate to severe hepatic impairment
- Alert for symptoms and signs suggestive of bone-marrow failure, such as anaemia, bruising, or infection. Seek immediate medical attention if rash or signs or symptoms of hypersensitivity syndrome develop
|
| 7. Clobazam |
- Drowsiness and lightheadedness the next day
- Confusion and ataxiaΩ (especially in the elderly)
- Amnesia
- Dependence
- Paradoxical increase in aggression
- Muscle weakness
- Visual disturbances
- Salivation changes
|
- Use with caution in patient with respiratory disease, muscle weakness and myasthenia gravisϒ (avoid if unstable), history of drug or alcohol abuse, marked personality disorder, acute porphyriaΦ.
- Contraindicated in respiratory depression, acute pulmonary insufficiency, sleep apnoea syndrome
- Seek immediate medical attention if symptoms such as rash, blistering or peeling of skin, sores in the mouth or hives develop
|
| 8. Clonazepam |
- Drowsiness (occurs in 50% of patients when starting drug)
- Muscle hypotonia, co-ordination disturbances
- Poor concentration, amnesia
- Dependence
- Restlessness, confusion
- Hypersecretion in infants and small children
- Nystagmusδ
|
- Use with caution in elderly and debilitated patients, patient with respiratory disease, airways obstruction, spinal or cerebellar ataxiaΩ , brain damage; history of alcohol or drug abuse, depression or suicidal ideation; myasthenia gravisϒ(avoid if unstable); acute porphyriaΦ, severe hepatic impairment.
- Contraindicated in respiratory depression, acute pulmonary insufficiency, sleep apnoea syndrome, coma, current alcohol or drug abuse
|
| 9. Retigabine |
- Increased appetite and weight gain
- Nausea, constipation, dyspepsia, dry mouth
- Drowsiness, dizziness
- Dysuria
- Malaise
- Tremor, impaired coordination
- Confusion, anxiety
- Blurred vision, diplopia, discoloration of ocular tissue
|
- Use with caution in patient at risk of urinary retention and known cardiac conduction problem
- Reduce dose in hepatic and renal impairment
|
| 10. Topiramate |
- AtaxiaΩ
- Impaired concentration, confusion, difficulties with memory or cognition
- Dizziness, drowsiness
- Fatigue
- Agitation, mood disorder
- Nausea
- Visual disturbance
- Weight loss
- Renal calculi
|
- Use with caution in patient at risk of metabolic acidosis, or renal calculi (ensure adequate hydration), renal impairment, or moderate to severe hepatic impairment
- Avoid in acute porphyriaΦ
|
| Category 3 drug |
| 11. Gabapentin |
- Somnolence
- Dizziness
- AtaxiaΩ
- Fatigue
- Nausea and vomiting, dry mouth, dyspepsia, diarrhoea
- Weight gain, oedema
- Amnesia
- Pharyngitis, rhinitis
- Arthralgia, myalgia
- Confusion, depression, nervousness
|
- Use with caution in the elderly, patient with diabetes mellitus , history of psychotic illness, renal impairment, and in those undergoing haemodialysis
|
| 12. Pregabalin |
- Somnolence
- Blurred vision, diplopia
- Increased appetite and weight gain
- Dry mouth, constipation, vomiting, flatulence
- Euphoria, confusion
- Sexual dysfunction
- Impaired memory and coordination
|
- Use with caution in patient with severe congestive heart failure, and patient with conditions that may precipitate encephalopathy.
|
| 13. Vigabatrin |
- Drowsiness
- Fatigue
- Excitation and agitation (in children)
- Headache
- AtaxiaΩ and paraesthesia
- Impaired concentration and memory
- Weight gain and oedema
- Irreversible visual field defects
|
- Caution in the elderly; patient with history of psychosis, depression, or behavioural problems; absence seizure.
- Contraindicated in patient with visual field defects.
- Careful monitoring for any new visual symptoms that develop, and seek immediate medical attention if encountered
|
| 14. Levetiracetam |
- Somnolence
- Weakness
- Dizziness
- Anorexia
- Nausea
- Diarrhoea
- Weight changes
- AtaxiaΩ
- Tremor
- Insomnia
- Diplopia
- Alopecia
|
- Caution in patient with renal impairment, or severe hepatic impairment.
|
| 15. Lacosamide |
- Dizziness
- Headache
- Nausea
- Diplopia
- Depression
- Abnormal coordination
- Impaired memory
- Somnolence
- Tremor
- Blurred vision
- Vertigo
- Gastrointestinal disorders
|
- Caution in the elderly, or patient with severe cardiac disease (such as history of myocardial infarction or heart failure), severe hepatic or renal impairment.
- Contraindicated in cardiac conduction problem.
|
|
Ω - A lack of muscle coordination during voluntary movements, such as walking or picking up objects
# - Risk of severe skin reaction known as Stevens-Johnson syndrome in the presence of the allele
Φ - A metabolic disorder that results in build-up of porphyrin in your body, affecting nervous system and/or skin
ψ - Unwanted male-pattern hair growth in women
δ - Rapid back-and-forth shifting in the eyes
χ - Low platelet count
ϒ - Weakness and rapid fatigue of any of the muscles under your voluntary control
|
▲ back to top
Withdrawal
|
Avoid abrupt withdrawal, particularly of phenytoin, clobazam and clonazepam, as this can precipitate severe rebound seizures. Even in patients who have been seizure-free for several years, there is a significant risk of seizure recurrence on drug withdrawal.
AEDs should only be withdrawn under doctor’s supervision, and dosage should be gradually reduced as prescribed by the doctor.
|
|
|
▲ back to top
General advice on using AEDs
|
- Take the prescribed dose of an AED every day on a long-term basis to suppress seizure. Adherence to the drug regimen prescribed by your doctor is essential for the control of epilepsy. Never suddenly stop taking an AED because doing so could cause a seizure.
- Routine blood test is needed for certain drugs to monitor the adverse effects on internal organs, and to assess blood levels of drugs. Adhere to the blood test schedule as prescribed by your doctor.
- Avoid heavy drinking as it can cause seizure, as well as interact with AEDs, making them less effective. AEDs can heighten the effects of alcohol, while alcohol can make the side effects of AEDs worse.
|

|
- If you feel drowsy, you should not drive or operate machinery. Patient with epilepsy are legally prohibited from driving in Hong Kong.
- Get enough sleep as lack of sleep can trigger seizures. Be sure you get adequate rest every night.
- Exercise regularly as exercising may help keep you physically healthy and reduce depression. Make sure you drink enough water and take a rest if you get tired during exercise.
- Stress can trigger seizure for some people. Stress-relieving and relaxation therapies such as exercise, yoga and meditation may help.
|
|
▲ back to top
Communication with your doctor
|
|
- Communicate with your doctor for the best treatment option. Your doctor will prescribe the most appropriate drugs for you after considering your condition and your response to the drugs.
- Watch out for any unusual and serious side effects that develop. If you experience any such symptoms, contact your doctor immediately.
- Notify your doctor immediately if you notice new or increased feelings of depression, suicidal thoughts, or unusual changes in your mood or behaviour.
- Inform your doctor of your medical history, as some diseases may warrant special precautionary measures.
|
|
 |
- Do not take other medicines, including over-the-counter medicines or complementary medicines such as St. John’s Wort, without first speaking to your doctor. Other medicines could have a dangerous interaction with your AEDs and cause a seizure.
- If you are planning a pregnancy, you should discuss with your doctor the impact of both epilepsy, and its treatment, on the outcome of pregnancy as there is an increased risk of serious birth defect associated with the use of AEDs. Your doctor may change your AED to minimise the risk.
- Tell your doctor if you are breast-feeding. Doctor will assess if the infant needed to be monitored for some side effects of drugs, especially if you are taking more than one AED.
|
|
▲ back to top
Storage of AEDs
AEDs should be kept in a cool and dry place. Unless specified on the label, medicines should not be stored in refrigerators. Furthermore, drugs should be kept properly in places unreachable by children to prevent accidental ingestion.
|
|
▲ back to top
|
|
Acknowledgement: The Drug Office would like to thank the Professional Development and Quality Assurance (PD&QA) for their valuable contribution to the preparation of this article.
|
|
|
|
|