| |
Oral Antiosteoporotic Drugs
|
 |
Introduction
|
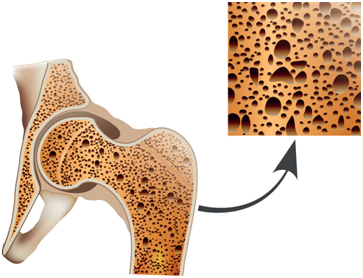
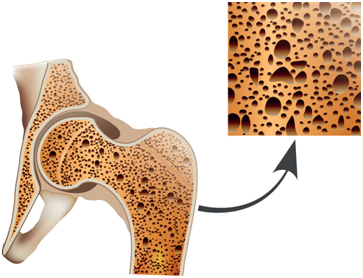
| Our bones (skeleton) build up a “hard” framework for our body; however, when we get older, our body framework may become “brittle” and we may unintentionally tumble down to sustain serious injuries and consequences. One of the major causes is depletion of calcium from the bone. Our bone becomes “less strong” when the mineral density of the bone is lower than normal, and in a more severe scenario, a disease state of “osteoporosis” could result. |
|
▲ back to top
Osteoporosis
|
Osteoporosis is a metabolic disease of the bone which leads to a reduction in bone mineral density (BMD), making your bone weak and brittle – so brittle that a fall or even mild stresses like bending over or coughing can cause a fracture. Worldwide, 1 in 3 women and 1 in 5 men over 50 years old will experience osteoporotic fractures. Osteoporotic fractures most commonly occur in the hip, wrist or spine. Spinal fractures cause stooped posture, loss of height, and chronic back pain. Hip fractures, the most serious consequences of osteoporosis, can result in permanent disability and even death.
|
Bones can adjust to the changing demands placed on them, and are continuously broken down and remodelled. In this process, small areas of bone tissue are removed and new bone tissue is deposited. Because more bone is formed than is broken down in the young adult years, bones progressively increase in density until about age 30, when they are at their strongest. After that, as breakdown exceeds formation, bones slowly decrease in density. Women lose bone mass rapidly in the first few years after the menopause due to lowered sex hormone levels. Losing bone mass is a normal part of the ageing process, but for some people it can lead to osteoporosis and an increased risk of fractures. Other factors that increase your risk of developing osteoporosis include inflammatory conditions such as rheumatoid arthritis, chronic obstructive pulmonary disorder, a family history of osteoporosis, long-term use of certain medications that affect bone strength or hormone levels such as oral steroid, malabsorption problems, and heavy drinking and smoking.
|
| In Hong Kong, hip and/or vertebral fractures due to osteoporosis is a major health concern, especially to the elderly people. A sedentary lifestyle with few outdoor activities, and low calcium intake in diet are some of the contributing factors for osteoporosis. |
|
|
▲ back to top
Diagnosis of osteoporosis
|
|
Although a diagnosis of osteoporosis is based on the results of your bone mineral density scan (with “dual-energy X-ray absorptiometry”, abbreviated DEXA or DXA), the decision of whether treatment is needed will be based on a number of factors including age, gender, risk of fracture and history of previous injury.
|
|
▲ back to top
Treatment of osteoporosis |
Before initiating drug treatments, lifestyle change (e.g. suitable exercise, regular diet, and outdoor sunshine) may help in mitigating the condition of osteoporosis.
Lifestyle “treatment”
Lifestyle changes will be needed as they affect how healthy your bones are. Regular exercise such as weight-bearing and resistance exercises, healthy diet with sufficient calcium and vitamin D, limiting alcohol intake and quitting smoking can help to prevent osteoporosis.
Maintain a sufficient daily intake of calcium and vitamin D is recommended. Vitamin D is absorbed from the diet but can also be manufactured in the skin using sunlight. Your body needs vitamin D to absorb calcium from food and incorporate it into bones.
Drug treatment
Anti-osteoporotic drugs not only increase bone mass, but also significantly reduce the risk of fracture. Drug treatments are better fitted with a lifestyle modification.
Registered anti-osteoporotic drugs in Hong Kong are in oral dosage forms (e.g. bisphosphonate tablets or calcitriol capsules) or injectable form (e.g denosumab, teriparatide). All of them are prescription-only medicines and must be administered strictly under doctor’s instruction.
|

|
|
|
▲ back to top
Oral antiosteoporotic drugs |
Commonly used oral anti-osteoporotic drugs include:
- Bisphosphonates: They slow down the rate of the bone being broken down. It helps to maintain the overall density of the bones and reduces the risk of bone fracture. Examples include alendronate and risedronate.
- Selective oestrogen receptor modulator (SERM): It has similar effect on bone as oestrogen. It helps by gradually reversing the excessive breakdown of bones, which usually happens after menopause. For SERM, Raloxifene is the only drug that is available for treating and preventing osteoporosis in post-menopausal women.
- Calcitriol: It is a high potency vitamin D analogue. It promotes the absorption of calcium and phosphate which are the two crucial materials for bone structure formation. The drug is used for the treatment of established post-menopausal osteoporosis.
|
 |
In general, a bisphosphonate (e.g. alendronate, risedronate) is recommended as first-line treatment for osteoporosis. Raloxifene (for women only) is an alternative if a bisphosphonate is contra-indicated or not tolerated. Calcitriol is prescribed for established post-menopausal osteoporosis.
When starting anti-osteoporotic treatment, your doctor may also give you calcium and vitamin D supplements if you are not getting enough from your diet.
On the market, there are two kinds of vitamin D preparations. Calcitriol is a vitamin D analogue which requires a doctor’s prescription. On the label of a prescription-only medicine such as calcitriol, you will notice the text “Prescription Drug 处方药物”. Other commonly used vitamin D3 containing supplements can be purchased over the counter.
|
|
|
▲ back to top
Common side effects and precautions
Antiosteoporotic drug
|
Common side effects
|
Precautions
|
| 1. Bisphosphonate |
- Nausea
- Abdominal pain
- Flatulence
- Change of bowels
- Difficulty swallowing
- Musculoskeletal pain
- Headache
|
- Take drug on an empty stomach (usually first thing in the morning) in an upright posture with a full glass of water. Avoid food and maintain an upright posture for at least 30 minutes after taking the drug.
- Report any thigh, hip, or groin pain during treatment.
- Have dental examination before starting bisphosphonate as the drug may affect jawbone.
- Be aware of any symptoms (e.g. pain or infections) in the ears, especially when using bisphosphonates with other drugs (such as steroids, or anti-cancer drugs) because the bisphosphate drugs may increase the risk of ear canal bone problem (osteonecrosis).
- Contraindicated in hypocalcaemia, active peptic diseases, and oesophageal abnormalities (such as reflux, oesophagitis, oesophageal stricture or achalasia); and it should not be used with known history of hypersensitivity to the drug.
- Use with caution in renal impairment.
|
| 2. Raloxifene |
- Hot flushes
- Leg cramps
- Peripheral oedema
- Influenza-like symptoms
|
- Contraindicated in patients with history of venous thromboembolism, undiagnosed uterine bleeding, endometrial cancer, cholestasis, or known hypersensitivity.
- Avoid use in hepatic impairment
- Use with caution in mild to moderate renal impairment, avoid in severe impairment
|
| 3. Calcitriol |
- High blood calcium level (hypercalcaemia)
- Headache
- Abdominal pain, nausea
- Rash
- Urinary tract infection
|
- Contraindicated in patients with diseases of high blood calcium level (hypercalcaemia), evidence of metastatic calcification, vitamin D toxicity; or hypersensitivity.
- During treatment of calcitriol, all other vitamin D supplements (including vitamin D fortified foodstuff) should be withheld.
- Be aware of any signs of hypercalcaemia (e.g. headache, vomiting, constipation, and loss of appetite). Very high levels of calcium in blood may result in fever, thirsty, extra urine, stomach pain, or uneven heart beat.
- Have adequate fluid intake, and avoid dehydration.
- Tell your doctors if you are also taking other drugs (such as thiazide diuretics, antacids, or digitalis).
|
|
|
▲ back to top
General advice
|
- Maintain a healthy lifestyle:
- Do not smoke. Smoking increases the rate of bone loss and the chance of fracture.
- Avoid excessive alcohol. Consuming too much alcohol may decrease bone formation and increase fall risk.
- Exercise regularly. Adult aged 19 to 64 years should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity every week, such as cycling or fast walking. Weight-bearing exercise and resistance exercise such as running and Tai Chi are useful for improving bone density and prevention of osteoporosis.
- Eat a healthy balanced diet with adequate calcium and vitamin D. Calcium is important for maintaining strong bones. You are recommended to take at least 700mg a day, which is about the equivalent of one pint of milk. Other calcium-rich foods include green leafy vegetables, dried fruit, tofu and yoghurt.
|
 |
|
- Take precautions to prevent falls:
- Wear low-heeled shoes with non-slip soles.
- Check your house for obstacles that might cause you to trip or fall, including electrical cords, area rugs and slippery surfaces.
- Keep rooms brightly lit to prevent falls.
- Put on glasses or hearing aid if needed to ensure you are responsive to the environment.
- Expose to sunlight: Sunlight stimulates the production of vitamin D, which helps your body absorb calcium. Short exposure to sunlight without wearing sunscreen (10 minutes twice a day) should provide you with enough vitamin D.
|
|
|
|
▲ back to top
Communication with your doctor
|
|
- Discuss with your doctor before starting a new exercise programme to make sure it is suitable for you.
- Do not take any drugs that can make you drowsy or that may lower your blood pressure too much and increase your risk of falls. Discuss with your doctor if you have drowsiness that may be related to the drugs that you are taking.
- Communicate with your doctor for the best treatment option. Your doctor will prescribe the most appropriate drugs for you after considering your condition and your response to the drugs.
- Attend follow-up medical appointment as scheduled. The need to continue anti-osteoporotic medication should be re-evaluated by your doctor periodically based on the benefit of your treatment.
- Watch out for any unusual and serious side effects that may develop. If you experience any such symptoms, contact your doctor immediately.
- Inform your doctor of your medical history, as some diseases may warrant special precautionary measures.
|
 |
|
|
|
▲ back to top
Storage of Antiosteoporotic drugs
Anti-osteoporotic drugs should be kept in a cool and dry place. Unless specified on the label, medicines should not be stored in refrigerators. Furthermore, anti-osteoporotic drugs should be kept properly in places unreachable by children to prevent accidental ingestion.
|
|
▲ back to top
|
|
Acknowledgement: The Drug Office would like to thank the Professional Development and Quality Assurance Service (PDQAS) for their valuable contribution to the preparation of this article.
|
|
|
|
|