| |
Glaucoma Drugs
|
 |
What is glaucoma?
|
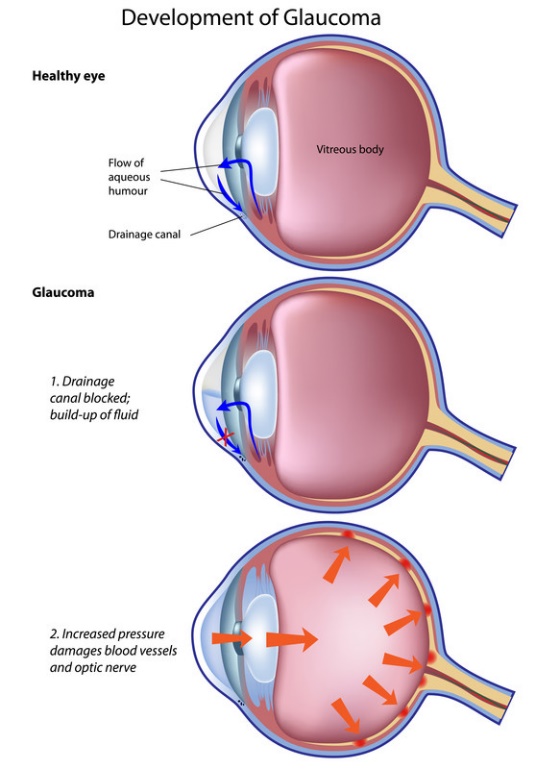
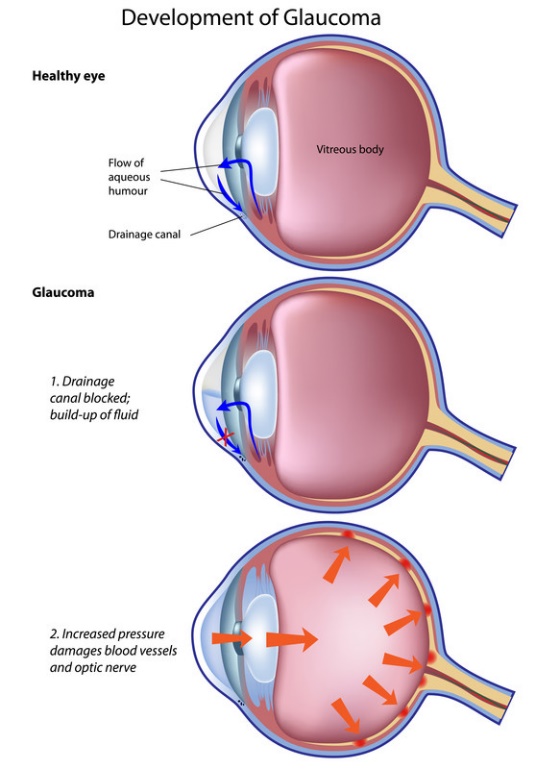
Glaucoma are eye conditions associated with damage of the optic nerve (which connects the eye to the brain) and the nerve fibres from the retina (the light-sensitive nerve tissue that lines the back of the eye). Glaucoma often affects both eyes, usually to varying degrees. If left untreated, glaucoma will cause progressive loss of outer field of vision (peripheral vision), then developed tunnel vision, and resulted in permanent total blindness.
|
Glaucoma is usually caused by abnormally high pressure inside the eye (intraocular pressure), but can be happened with normal intraocular pressure. Glaucoma is described as open-angle or angle-closure, depending on the mechanism of the obstruction of drainage. |
In open-angle glaucoma, the drainage angle formed by the cornea and the iris remains open, but the drainage channels (trabecular meshwork) in the angle are partially blocked, causing the fluid (aqueous humor) to drain out of the eye slowly. This causes fluid to back up in your eye, and pressure gradually increases within your eye. The condition is often asymptomatic. Vision is lost gradually from the outer rim of the eye, slowly working inwards towards the centre. |
Angle-closure glaucoma occurred when the iris bulges forward to narrow or block the drainage angle formed by the cornea and the iris. Fluid can't adequately flow through and exit the eye, leading to an increase in eye pressure. Angle-closure glaucoma usually occurs suddenly (acute angle-closure glaucoma), but it can also occur gradually (chronic angle-closure glaucoma). Symptoms of acute angle-closure glaucoma include intense eye pain, tender eye area, nausea, vomiting, headache, sudden onset of visual disturbance (often in low light), blurred vision, halos (circles) around lights and reddening of the eye. Symptoms of acute glaucoma are not constant. They can last for one or two hours before disappearing again. But each time the symptoms occur, your vision is damaged a little more. |
Both open-angle or angle-closure glaucoma can be primary or secondary. Primary glaucoma usually associated with a direct disturbance of fluid outflow. Secondary glaucoma develops as a consequence of some conditions or medications used, such as eye injury, uveitis (inflammation of the middle layer of the eye), tumor, advanced cataract, diabetes or long-term corticosteroid use. |
The risk factors for getting glaucoma are older age over 40, severe short sightedness, ocular hypertension, family history of glaucoma, diabetes and hypertension etc. People of Asian origin are at increased risk of developing acute angle-closure glaucoma and people of African or Afro-Caribbean origin are at increased risk of developing chronic open-angle glaucoma. |
|
|
▲ back to top
Treatment of glaucoma |
 |
Glaucoma cannot be cured and damage produced cannot be reversed. But if detected early and treated appropriately, further damage to vision may be prevented or delayed. Treatment aims to control the condition and minimize future damage. Currently, the most effective way of treating glaucoma is to decrease the intraocular pressure by using glaucoma drugs, laser treatment, eye surgery or a combination of these based on the patient’s type of glaucoma, severity, medical history and health conditions. The mechanisms involved are mainly through improving drainage of fluid in the eye or lowering the amount of fluid produced in the eye.
Acute angle-closure glaucoma develops rapidly, so the condition needs to be treated quickly. Besides topical eye preparations and systemic medicines to quickly reduce the pressure in your eye, laser iridotomy which uses high-energy beams of light to create holes in your iris and enable fluid to flow, or other surgery may be used. If you also have a cataract, removing it may open the angle in the eye and increase the outflow of the fluid so as to reduce the intraocular eye pressure.
|
|
|
▲ back to top
|
Classes of glaucoma drugs |
Topical beta-blockers
Topical application of a beta-blocker to the eye reduces intraocular pressure probably by reducing the rate of production of the fluid in the eye. Beta-blockers used as topical eye preparations include betaxolol, carteolol, levobunolol, and timolol.
Topical prostaglandin analogues and prostamides
The prostaglandin analogues latanoprost, tafluprost, and travoprost, and the synthetic prostamide, bimatoprost, increase outflow of aqueous humor and subsequently reduce intraocular pressure.
|
Topical alpha2-adrenoceptor agonists
Brimonidine, a selective alpha2-adrenoceptor agonist, is thought to lower intraocular pressure by reducing aqueous humor production and increasing its outflow.
|
Topical or oral carbonic anhydrase inhibitors
The carbonic anhydrase inhibitors, acetazolamide, given by mouth as well as topical brinzolamide and dorzolamide reduce intraocular pressure by reducing aqueous humor production. Systemic use of carbonic anhydrase inhibitors also produces weak diuresis.
|
|
Topical miotics
Miotics, e.g. pilocarpine increase the outflow of aqueous humor.
|
|
Intravenous hypertonic mannitol
Intravenous hypertonic mannitol is an example of osmotic diuretics which reduce vitreous volume and can produce a marked reduction in intraocular pressure. They are usually used in the short-term management of glaucoma.
|
|
Most of the registered glaucoma drugs in Hong Kong are available in topical forms e.g. eye drops, some of them are also available in tablets and injections. Combination of different ingredients may be prescribed and there are also topical eye preparations containing two active ingredients available.
|
|
Most of the glaucoma drugs are prescription-only medicines in Hong Kong.
|
|
|
|
▲ back to top
Common side effects and precautions of glaucoma drugs
Glaucoma drugs
|
Common side effects
|
Precautions
|
| 1. |
Topical beta-blockers |
- Ocular stinging, burning, pain, itching, erythema, dryness
- Allergic reactions including anaphylaxis and blepharoconjunctivitis
|
- Should be used with caution in patients with corneal diseases, stable heart failure, first-degree atrioventricular block (AV block), diabetes
- Should not be used in patients with bradycardia, heart block, or uncontrolled heart failure, asthma or a history of obstructive airways disease, frequent episodes of hypoglycaemia, breastfeeding, metabolic acidosis, cardiogenic shock, hypotension, severe peripheral arterial disease, sinus bradycardia, and second- or third-degree AV block
|
| 2. |
Topical prostaglandin analogues and prostamides |
- Changes in blood pressure
- Headache
- Ocular discomfort
- Conjunctival disorders
- Brown pigmentation particularly in those with mixed-colour irides
- Blepharitis
- Pigmentation of periocular skin
- Eyelash and vellus hair changes (including darkening, thickening and lengthening of eye lashes)
- Reduced visual acuity
- Photophobia
- Punctate keratitis
- Transient punctate epithelial erosion
- Corneal erosion
|
- Should be used with caution in patients with aphakia, pseudophakia with torn posterior lens capsule or anterior chamber lenses, and in those with known risk factors for cystoid macular oedema, iritis, uveitis, or a history of significant ocular viral infections
- Care is also needed in patients with chronic obstructive pulmonary disease, asthma or compromised respiratory function. There is no experience of use in inflammatory ocular conditions, neovascular, angle-closure glaucoma, congenital glaucoma, or narrow-angle glaucoma
- Possible change in eye colour as an increase in the brown pigment in the iris can occur, which may be permanent; particular care is required in those with mixed coloured irides and those receiving treatment to one eye only
- Changes in eyelashes and vellus hair can also occur, avoid repeated contact of the eye drop solution with skin as this can lead to hair growth or skin pigmentation
|
| 3. |
Topical brimonidine, a selective alpha2-adrenoceptor agonist |
- Dry mouth
- Gastro-intestinal disturbances
- Taste disturbances
- Upper respiratory symptoms
- Headache
- Drowsiness
- Dizziness
- Malaise
- Ocular disturbances (including hyperaemia, burning, stinging, pruritus, pain and dryness)
- Visual disturbances
- Eyelid inflammation
- Photophobia
- Corneal erosion and staining
- Conjunctival disturbances (including blanching, follicles, and infection)
|
- Should be used with caution in severe cardiovascular disease; cerebral or coronary insufficiency, Raynaud's syndrome, thromboangiitis obliterans, postural hypotension, depression; children 2-12 years (increased risk of drowsiness), hepatic impairment, renal impairment, pregnancy
- Should not be used in neonate or child under 2 years and mother on breastfeeding
|
| 4. |
Topical brinzolamide and dorzolamide, carbonic anhydrase inhibitors |
Topical brinzolamide
- Taste disturbances
- Dry mouth
- Headache
- Ocular disturbances (including corneal erosion, corneal oedema, photophobia, and reduced visual acuity)
Topical dorzolamide
- Nausea
- Bitter taste
- Headache
- Asthenia
- Ocular irritation
- Blurred vision
- Lacrimation
- Conjunctivitis
- Superficial punctate keratitis
- Eyelid inflammation
|
Topical brinzolamide and dorzolamide
- Systemic absorption follows topical application and can rarely cause sulfonamide-like side-effects and may require discontinuation if severe
- Should not be used in hyperchloraemic acidosis, sulfonamide hypersensitivity, renal impairment with estimated glomerular filtration rate (eGFR) less than 30 mL/minute/1.73 m2, pregnancy
Topical brinzolamide only
- Should be used with caution in renal tubular immaturity or abnormality, renal impairment, breastfeeding
- Should not be used in hepatic impairment
Topical dorzolamide only
- Should be used with caution in history of renal calculi; chronic corneal defects, low endothelial cell count, history of intraocular surgery, hepatic impairment
- Should not be used in breastfeeding
|
| 5. |
Oral acetazolamide, carbonic anhydrase inhibitor |
- Nausea
- Vomiting
- Diarrhoea
- Taste disturbance
- Loss of appetite
- Paraesthesia
- Flushing
- Headache
- Dizziness
- Fatigue
- Irritability
- Excitement
- Ataxia (a lack of muscle coordination during voluntary movements, such as walking or picking up objects)
- Depression
- Thirst
- Polyuria
- Reduced libido
|
- Not generally recommended for prolonged use
- Should be used with caution in patients with pulmonary obstruction or pulmonary emphysema and impaired alveolar ventilation; elderly; diabetes mellitus; renal calculi
- Should not be used in hypokalaemia, hyponatraemia, hyperchloraemic acidosis; adrenocortical insufficiency; long-term administration in chronic angle-closure glaucoma; sulfonamide hypersensitivity; hepatic impairment, renal impairment, pregnancy, Addison's disease
- Blood disorders, rashes, and other sulfonamide-related side-effects occur occasionally — patients should report any unusual skin rash
|
| 6. |
Pilocarpine, topical miotics |
- Ciliary spasm leads to headache and browache which may be more severe in the initial 2–4 weeks of treatment (a particular disadvantage in patients under 40 years of age).
- Ocular side-effects include burning, itching, smarting, pain and irritation, lachrymation, blurred vision, conjunctival vascular congestion, myopia, lens changes with chronic use, vitreous haemorrhage, and increased pupillary block
|
- Should be used with caution in patients with peptic ulceration, gastro-intestinal spasm, cardiac disease, hypertension, hypotension, marked vasomotor instability, asthma, epilepsy, Parkinson's disease, hyperthyroidism, and urinary-tract obstruction and patients wearing soft contact lenses, dementia of Alzheimer type
- Should not be used in conditions where pupillary constriction is undesirable such as acute iritis, acute uveitis, anterior uveitis and some forms of secondary glaucoma. Should not be used in acute inflammatory disease of the anterior segment of the eye, pregnancy, breastfeeding
- Not commonly used for the treatment of primary open-angle glaucoma because side-effects, such as pupil miosis, are poorly tolerated for pilocarpine
- A darkly pigmented iris may require a higher concentration of the miotic or more frequent administration and care should be taken to avoid overdosage
- Care is required in conjunctival or corneal damage and retinal disease and in young patients with myopia
- Intraocular pressure and visual fields should be monitored in those with chronic simple glaucoma and those receiving long-term treatment with a miotic
- Blurred vision may affect performance of skilled tasks (e.g. driving) particularly at night or in reduced lighting
|
| 7. |
Intravenous hypertonic mannitol |
- Hypotension
- Thrombophlebitis
- Fluid and electrolyte imbalance
|
- Should be used with caution as extravasation causes inflammation and thrombophlebitis
- Should be used with cautions in severe renal impairment
- Should not be used in heart failure; severe pulmonary congestion or frank pulmonary oedema; intracranial bleeding (except during craniotomy); anuria; severe dehydration, pregnancy, breastfeeding
|
|
|
▲ back to top
General advice
|
-
Apply glaucoma topical eye preparations or take glaucoma medicines
regularly by following the prescription’s instruction exactly
even if you have no symptoms.
- Follow the instructions of using the preparations as labelled.
To minimize systemic side effects due to topical eye preparations absorbed
into your bloodstream, close your eyes for one to two minutes after putting
the medicines in, press lightly at the corner of your eye near your nose to
close the tear duct for several minutes, and wipe off any unused medicines
from your eyelid. For other skills of using eye drops please refer to How to
Use Eye Drops at
http://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/
popular_drug_usages/how_to_use_eye_drops.html.
|
|
 |
- Write down the date you need to discard the bottle/tube of topical eye preparations when you first opened a new bottle/tube based on the labelled period suggested on the box or that recommended by the healthcare professionals.
- Contact lenses should be taken out before instillation of some topical eye preparations and may be put back in the eyes 15 minutes after you have used the topical eye preparations.
- While eating a healthy diet won't prevent glaucoma from worsening, it can improve your physical and mental health. It can also help you maintain a healthy weight and control your blood pressure.
- Drinking one liter or more of any liquid within a short time may temporarily increase eye pressure. Thus drink only moderate amounts of fluids at any given time during the course of a day.
- Limit your caffeine as drinking high amounts of caffeine may increase your eye pressure.
- Sufficient rest and exercise are beneficial. Patients are also advised to optimize the cardiovascular risk factors so as to enhance the blood circulation at the optic nerve head. Talk to your doctor about an appropriate exercise programme.
- Serious eye injuries can lead to glaucoma. Wear eye protection spectacles when you use power tools or play high-speed racket sports on enclosed courts. Also wear hats and sunglasses if you spend time outside. Trauma should certainly be avoided especially in those who underwent glaucoma surgery.
- Practise healthy relaxation techniques to cope with stress as stress may trigger an attack of acute angle-closure glaucoma in patients at risk.
- If you have glaucoma, it could affect your ability to drive.
|
|
|
|
▲ back to top
Communication with your doctor
|
| |
 |
- If you have symptoms of acute angle-closure glaucoma or other forms of glaucoma, visit your doctor or go to the nearest accident and emergency (A&E) department immediately.
- A diagnosis of glaucoma generally means lifelong treatment and regular checkups to prevent further damage to your vision.
- Inform your doctor if you have allergies towards any medicines, foods, colourants, preservatives, etc, and your medical history including renal or hepatic impairment, as some diseases may warrant special precautionary measures.
|
- Tell your doctor if you are currently taking other drugs as the drugs may interact with glaucoma drugs. Moreover when visiting other physicians or buying other medicines in a pharmacy for other diseases, please tell the doctor or pharmacist if you are suffering from glaucoma and the names of glaucoma medications you are taking.
- Tell your doctor if you are pregnant or breastfeeding as some glaucoma drugs should be avoided.
- If you experience any unusual and serious side effects, some may not be listed above, contact your doctor immediately.
|
|
|
|
▲ back to top
Storage of glaucoma drugs
Store the drugs in accordance to that as labelled. The drugs should be kept in a closed container in a cool and dry place away from direct light. Unless specified on the label, medicines should not be stored in refrigerators. Furthermore, drugs should be kept properly in places unreachable by children to prevent accidental ingestion or application. Discard outdated medicine.
|
|
▲ back to top
|
|
Acknowledgement: The Drug Office would like to thank the Professional Development and Quality Assurance (PD&QA) for their valuable contribution to the preparation of this article.
|
|
|
|
|